Stereotactic biopsy
The goal of a stereotactic biopsy is to get a diagnosis from pathological processes where open surgery would be too risky. This mostly involves deep-seated or multifocal processes. Other indications are lymphomas, which often can be - due to proper diagnosis - treated without surgery by radiation / chemotherapy. Numerically rare inflammatory processes are biopsied. In all these processes, the accurate diagnosis is a prerequisite for further treatment by radiation, chemotherapy or targeted antibiotic therapy. The significance of stereotactic biopsy in tumors is over 90% with a complication rate of less than 5%. The most important complication is a clinically relevant bleeding. Thanks to the precise preoperative planning of access and extraction point the risk of bleeding becomes relatively low. Stereotactic biopsy represents a very gentle and safe procedure, which for over 30 years has been part of the neurosurgical standard.
In our Department during stereotactic biopsy at first the stereotactic base ring is attached to the patient skull - under anesthesia - and customized CT images are produced under stereotactic conditions. These are transferred to the computer. Through the sectional images, the sampling point is determined and its exact location in relation to the set base ring from the CT / MR images is accurately determined. The computer automatically calculates the angle which must be adjusted on the alignment bracket to reach the planned sampling point.
In the operating room the superimposed stereotactic ring is attached together with the patient to the operating table. At the Phantom the location and the arrival of the planned sampling point is controlled. Afterwards the insertion handle is transferred to the patient's ring. After opening the skull via a small hole, the biopsy needle is inserted. The cannula is curved and not sharp, so that during the advancement brain tissue and vessels are displaced, yet not injured. Subsequently, several samples are taken from different depths along the cannula path through the tumor, in order to get a representative picture of the histological structure of the pathological process. Figure 5 shows a biopsy cylinder of about 8mm in length. The samples are analyzed during the operation by the neuropathologist and he makes a preliminary diagnosis. As soon as sufficient representative material was removed, the needle is withdrawn and the operation ends. In the most cases the biopsy are endogenous brain tumors - so called gliomas - of different benignancy. Typically malignancy increases with increasing cell number and cell density. Figure 6 shows on the top left picture cell-poor benign form and on the right below the vicious cell-rich form of glioma. The final diagnosis with special staining methods requires about 1 week. Usually, the patient can be mobilized one day after the biopsy and discharged after a few days until the arrival of the final diagnosis.

Fig.5
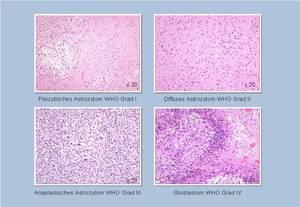
Fig.6
With the same method - as the stereotactic biopsy - deep-lying cysts or abscesses are punctured and deflated.




