Deep brain stimulation: Operation procedure
A few days before the operation, planning is carried out using current magnetic resonance images (MRI). In the case of Parkinson's disease typically electrodes have to be introduced into the subthalamic nucleus (STN) on both sides. The software enables to depict the target point in the STN within respective layers and to plan the access to avoid injury of vessels or important brain structures.
On operation day at first the stereotactic base ring is attached to the patient skull under general anesthesia and a CT is conducted under stereotactic conditions. These CT images are combined with the MR images on the computer and the coordinate of the target point is located in relation to the attached base ring. Simultaneously 4 angles and the needle depth can be calculated, which must be adjusted on the aiming arm to reach the target point.
In the meantime, the patient is fixed in the operating room via a terminal on the operating table with the base ring. On the Phantom it is checked whether the destination point will be reached exactly. Afterwards the insertion handle is transmitted to the base ring of the patient and a borehole is milled. The dura mater is opened. Now the sedation is turned off and when the patient is awake the breathing tube is removed.

Fig.8
Next, an extremely thin microelectrode is inserted, just before the target point. This is not painful because the brain itself has no pain sensitivity. The microelectrodes are used to record the electrical activity around the needle tip. Registration happens at 1mm-2mm increments of 10mm before to about 3mm above the calculated target point. The STN has a characteristic pattern of neural activity. The derivation confirms the correct position of the microelectrode tip. With the same microelectrode in each depth an electrical stimulation is caused with increasing current. The neurologist present registers the effect and potential side effects for each setting. From the combined effect of all the collected data, the optimal location for the final electrode position is determined. After removal of the microelectrode, the final electrode is inserted and the location is controlled with X-rays. The electrode itself has 4 contacts at the tip, which can be connected to one another as desired. This increases the flexibility and allows an optimal patient-adapted programming after implantation. The final electrode is attached to a plastic cap that fits exactly into the well. In case of Parkinson's disease the same procedure on the opposite side is performed. There are 2 options: Either you implant the pacemaker in the same session and connect the electrodes via connecting cables to the pacemaker, or a few days later you decide to perform this peacemaker implantation in a separate procedure under anesthesia. The pacer is typically implanted in the chest, just under the skin below the collarbone.

Fig. 9
After surgery, the patient is taken to neurosurgical ward for 1-2 days. Before transferring to the Department of Neurology, a control CT is performed to rule out complications and to check the position of the electrodes. The correspondence between the planned and the current electrode layer can be checked by using the planning station (Fig.10).
The Department of Neurology then fine tunes the stimulation parameters and the patient learns how to start and turn off his pacemaker with an own device and modify some stimulation parameters as needed.
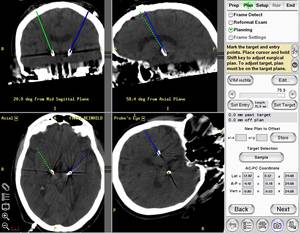
Fig.10
Contact Stereotaxis
Neurosurgical Team:
OÄ Dr. med. Dörthe Keiner
Phone: 06841-1614450
Email:Doerthe.Keiner @uks.eu
Prof. Dr. med. Peter Grunert
Phone: 06841/16 24451 oder 06841/16 24100
Email:Peter.Grunert @uks.eu
Registration for Admission:
Sr. Susanne Mathieu
Phone: 06841/16 24421
Neurological Team:
Prof. U. Dillmann, PD J. Spiegel, OA J. Bürmann
available via ambulance for Parkinson´s disease
Phone: 06841/16 24138
or EMG 06841/16 24116




