Gliomas
General Information
Gliomas are primary brain tumors that originate from glial cells. These provide the supporting and nutritive tissue of the nerve cells. Depending on the cells of origin, one distinguishes different gliomas, such as Astrocytomas, Oligodendrogliomas, Ependymone or mixed forms as Oligoastrocytoma. Gliomas account for about 45-50% of intracranial tumors. Approximately 50% of gliomas are glioblastoma (astrocytoma WHO grade IV). Astrocytomas (WHO grade I-III) represent about 25% of gliomas and oligodendrogliomas less than 5-18% and Ependymomas account for 2-9%. Gliomas can occur in all areas of the brain and in rare cases, the spinal cord or the eye socket.
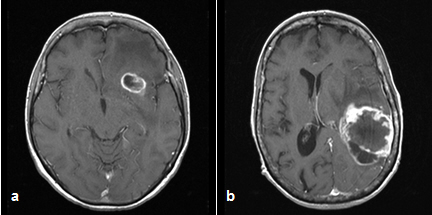
Depiction of glioblastoma on the MRI at different locations:
front left (a) and temporoparietal left (b)
Classification
As it is common for brain tumors, gliomas are classified according to the WHO classifications, which is based on the histological findings, the growth behavior, the likelihood of recurrence and thus the prognosis.
- WHO ° I: Tumor is histologically benign and curable by complete removal, usually relapse unlikely (e.g. pilocytic astrocytoma, ependymoma)
- WHO ° II: Tumor is histologically benign, but infiltrative growth and tendency to relapse, survival is not significantly reduced (e.g., diffuse astrocytoma, oligodendroglioma and slow-growing Oligoastrocytoma)
- WHO ° III: tumor is histologically malignant, survival time is limited (e.g. anaplastic astrocytoma, anaplastic ependymoma, anaplastic oligodendroglioma, anaplastic oligoastrocytoma)
- WHO ° IV: tumor is highly malignant, aggressive growth, survival time significantly reduced (e.g. glioblastoma)
Symptoms depend largely on the location of the tumors and its growth rate. It can cause intracranial pressure (e.g. headache, fatigue, nausea, and dizziness), neurological deficits (e.g. paralysis, impaired vision, gait, speech disorders) or epileptic seizures. In addition, there may be psychological changes such as disorientation or slight irritability.
The diagnosis is made by CT and MRI imaging. These images can also be used during surgery for neuronavigation to localize the tumor and surrounding brain structures accurately. For differential diagnosis radiological tests such as PET (positron emission tomography) or SPECT (single photon emission computed tomography) may be used as well. Depending on the location even more preoperative examinations such as navigated transcranial magnetic stimulation (NTMs) or diffusion tensor imaging Fibre-Tracking (tractography) might make sense.
The therapy depends on the cell type and the location of the tumor, the age and general condition of the patient and must be defined for each patient individually. It is determined by interdisciplinary collaboration with other participating disciplines, for example the Department of Radiotherapy or the Department of Internal Medicine I and coordinated with the patient. The main neurosurgical treatment is usually surgical removal of the tumor. This takes place via microsurgical techniques, and usually with the help of neuronavigation and various techniques of intraoperative monitoring as electrophysiological studies, fluorescence representation of the tumor tissue with 5-ALA, wax operations as well as intra-operative CT or ultrasound imaging.
In some cases, astereotactic biopsy can be useful to confirm the diagnosis before tumor removal. Depending on the type of tumor and the resection, surgical removal may be followed by a post-treatment. In the case of glioblastoma this means a subsequent combined radio- and chemotherapy. In case of recurrences a locally effective chemotherapeutic agent can beintroduced intraoperatively into the resection cavity.
Molecular-biological examinations of the tumor tissue can predict how well the different therapies can function in certain types of tumors. Thereby the therapy plan can be created more accurately and individually. This is also a key focus of our neuro-oncological research.
Our Expertise
- Complete spectrum of neurooncology and surgical options
- Close interdisciplinary cooperation with the Department of Radiation Therapy, Clinic of Internal Medicine I etc.
- Participation in oncological tumor board
- Neurooncological research
Medical Contact Person
OA PD Dr. med. R. Ketter
Email: Ralf.Ketter @uks.eu
HSA-Consultation Hours:
Tuesday 9am-2pm
Registration
HSA-Consultation Hours:
Tel.: 06841-1624412




